# Neuro-Ophthalmology
The most common ophthalmic manifestations of neurologic disease are abnormal pupil sizes, abnormal pupillary light responses (PLRs), and blindness. Menace responses and PLRs should be done on all ophthalmic examinations. Less commonly seen are abnormalities of eyelid position or abnormal position of the eyeball itself; we will not discuss either of these.
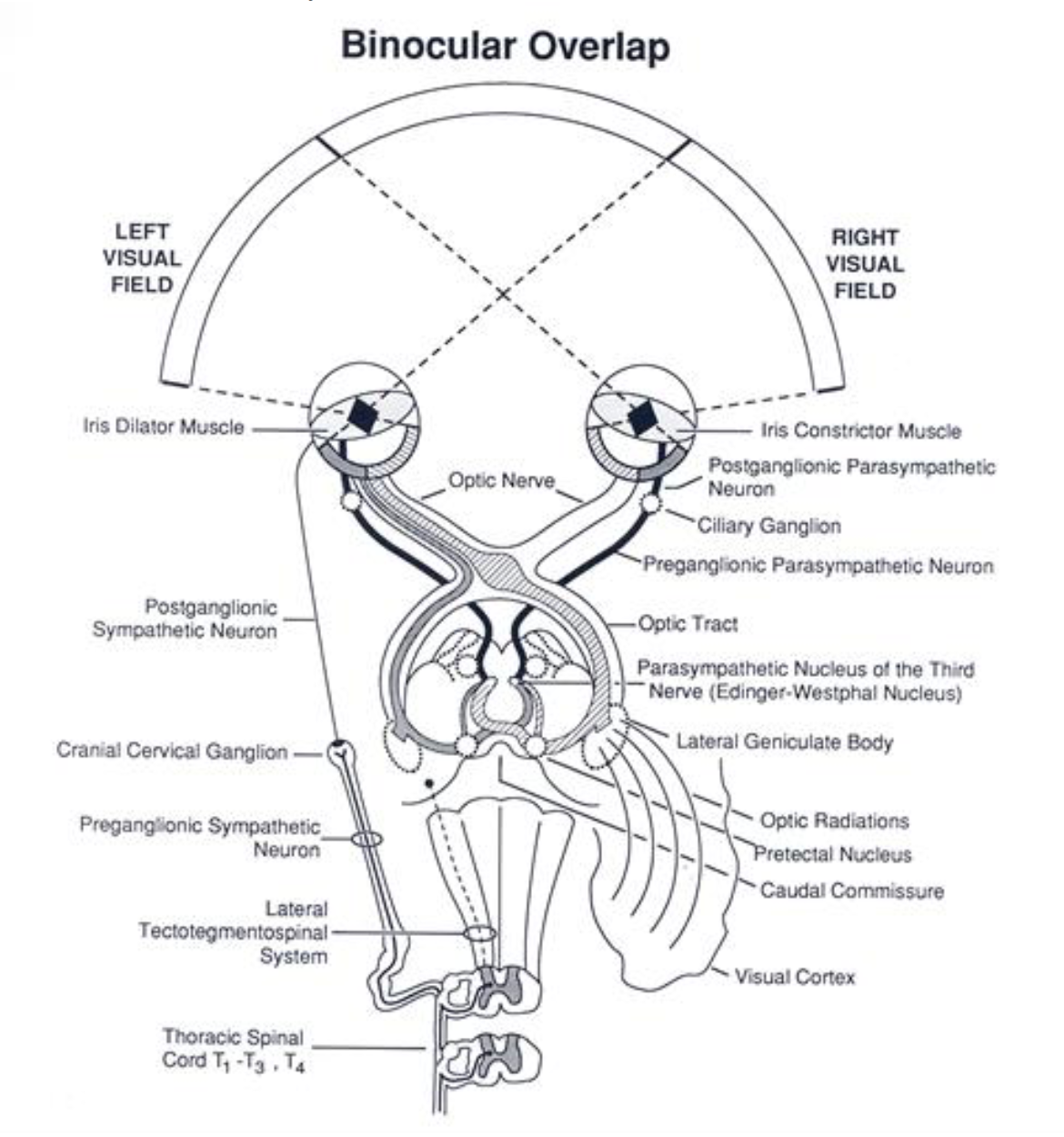
The primary receptors for the pupillary response and vision are the rods and cones from which electrical impulses pass to bipolar cells. From bipolar cells, impulses continue to retinal ganglion cells, the axons of which constitute the optic nerve. At the optic chiasm, part of the nerve fibers decussate (cross over); in most mammals, the fibers from the lateral part of the retina do not decussate much. The fibers continue from the optic chiasm as optic tracts (same axons). In the optic tracts, visual and pupillary fibers begin to differ in pathways.
The visual fibers synapse in lateral geniculate bodies and travel via optic radiations to the occipital cortex. The pupillary fibers continue to the midbrain to synapse in the pretectal nuclei (crossing occurs between the nuclei of the two sides). The pretectal nuclei fibers project and synapse in the oculomotor nuclei (both oculomotor nuclei receive axons of neurons from each pretectal nucleus). Preganglionic parasympathetic axons of the oculomotor nerve synapse in both ciliary ganglia. Postganglionic parasympathetic fibers innervate the iris sphincter and ciliary muscles.
Sympathetic innervation of the iris is necessary to provide control of pupil size by providing constant antagonism to the sphincter via the dilator muscle. The sympathetic impulses originate in the hypothalamus and rostral midbrain, pass to and synapse in the intermediate gray column of the first three thoracic segments of the spinal cord. Preganglionic sympathetic neurons pass to the thoracic sympathetic trunk, go cranially (usually without synapse in the intervening cervicothoracic and middle cervical ganglia) to enter the cervical sympathetic trunk. At the cranial cervical ganglion synapse occurs and postganglionic fibers concerned with pupil size pass to the dilator muscle of the iris (note: some sympathetic fibers have been found in the sphincter muscle and probably have an inhibitory function).
Be aware!! There are several non-neurologic causes of abnormal pupil sizes and/or PLRs. The most common examples are iris atrophy and synechia. Make sure you can differentiate these disorders from neurologic causes of pupillary abnormalities.
# Essentials of Neuroophthalmic Examination
Pupillary Light Response:
Direct - Response of pupil when light is shone in that eye.
Consensual - Response of pupil when light is shone in opposite eye.
Swinging flashlight test - Shine light in OS wait 2-3 seconds for pupils to constrict quickly bring light over to OD if OD was already constricted, then consensual OD was normal. If OD was not constricted, consensual OD not normal. If the OD pupil was constricted, it will not redilate in the short amount of time it takes to move the light from OS to OD.
Menace Response
- The menace response is present at birth (or within 1-2 weeks) in horses and other prey animals. It is a learned response in puppies and kittens, and therefore maybe absent in normal young predators until learned (about 7-8 weeks). When making the menacing gesture, avoid air movements and touching hair on the face.
Dazzle Response
- This is the involuntary avoidance response to a light shone into the eye. Especially when a strong light is directed at the eye, there will be blinking and possibly retraction of the globe with protrusion of the third eyelid and sometimes movement of the head away from the light. Although the neuroanatomical pathway for this response is not completely understood it is thought that the optic tract axons synapse in the rostral colliculus. A positive response generally is considered to be evidence of fundamental continuity of the eye to brain pathway and is suggestive that there may be the ability for vision. The presence of complete cataracts or corneal scarring would not be expected to prevent this response.
Cotton Ball Test
- A cotton ball is thrown in the line of sight and tracking is evaluated.
Maze Test
- Observe animal as it ambulates off leash around exam room with obstacles created from chairs, trash cans, etc.
# Neuroophthalmic Diseases
# Horner’s Syndrome
Definition:
Lack of sympathetic innervation to the eye and orbit.
Clinical signs / history:
Signs generally unilateral
Miosis (but direct and consensual PLRs are positive)
Enophthalmia
Protrusion of the third eyelid
Ptosis of the upper lid
May have history of trauma
Review sympathetic pathway to eye
Etiologies:
Any lesion of the sympathetic pathway can cause Horner’s syndrome.
Otitis media
Neck trauma (leash, dog fight)
Idiopathic – about 70% of Horner’s cases in dogs fall in this category
Diagnosis:
Appropriate collection of clinical signs
Pharmacologic localization to detect post-ganglionic lesions; phenylephrine most reliable
Pharmacologic localization only partly accurate due to unpredictable penetration of cornea by drugs. Additionally, denervation hypersensitivity takes days to weeks to develop.
Phenylephrine test
Apply one drop of 10% phenylephrine to each eye (the normal eye is serving as control)
Observe pupils every 10-20 minutes
Phenylephrine will dilate a normal pupil within about 1-2 hours, but will dilate a pupil with postganglionic (i.e., third order) Horner’s much faster, usually within 20-30 minutes
Should always do deep cervical palpation and flexion, as well as otic exam.
Consider MRI, chest films in selected cases.
Treatment:
Treat otitis if discovered.
Otherwise, leave alone; many cases resolve in weeks to months
# Dysautonomia
Definition:
Loss of autonomic innervation; includes systemic as well as ocular dysfunction, and sympathetic as well as parasympathetic.
Clinical signs / history:
Bilateral
Regurgitation (megaesophagus)
Constipation
Fecal and urinary incontinence
Decreased STT
Dilated nonresponsive pupils
Third eyelid protrusion
Etiology
- Unknown; was seen as an epidemic in early ‘80’s in Britain, and another more recent epidemic in hunting dogs in Kansas. Postulated environmental, infectious causes.
Diagnosis:
Proper spectrum of clinical signs.
Dilute pilocarpine to evaluate for parasympathetic denervation hypersensitivity of pupil
Treatment:
- Supportive for dry eye, regurgitation, and constipation.
Prognosis very poor.
# Cortical Blindness
Definition:
- Inability to see due to lesion of visual cortex.
Clinical signs/history:
Usually have other neurologic signs of cortical disease (seizures, ataxia, etc.)
PLRs normal
Etiologies:
Infectious
Neoplastic
Vascular
Hydrocephalus
Diagnosis:
- Blindness with normal PLRs
Treatment:
- Treat underlying brain disorder
Exercise: Localize the lesion
| Clinical signs | Site of Lesion |
|---|---|
Blindness OS, negative direct PLR OS, negative consensual PLR OD | |
Blindness OS, negative direct PLR OS, negative consensual PLR OD, positive ERG OS, negative VEP OD, ERG and VEP positive OS | |
Blind OU, negative direct and consensual PLR OU | |
Visual OU, negative direct and consensual PLR OD, positive direct and consensual PLR OS | |
Blind OU, positive direct and consensual PLR OU |