# Anterior Uveal Anatomy and Physiology
Anterior uvea is comprised of the iris and ciliary body which are extremely vascular
Iris contains the sphincter muscle, dilator muscle, and stroma
Ciliary body is made of the ciliary body muscle for accommodation and a pigmented and nonpigmented epithelium. The nonpigmented epithelium is thought to be responsible for creating aqueous humor.
Pupillary size and response to light (pupillary light reflex, PLR) are important to observe. A direct PLR describes how that pupil behaves when you shine a light into that eye. A consensual PLR describes how the pupil behaves when you shine a light into the opposite eye. PLRs should be brisk and complete.
In a normal eye, pupil size is a balance between the tonic activity of the parasympathetic nervous system activating the pupillary sphincter muscle, and the tonic activity of the sympathetic nervous system activating the pupillary dilator muscle. Also in a normal eye, light falling on the retina activates photoreceptors, which then activate a reflex pathway involving midbrain structures that loop back through the parasympathetic pathway to cause the pupil to constrict.
# Congenital abnormalities
# Persistent pupillary membranes
Definition
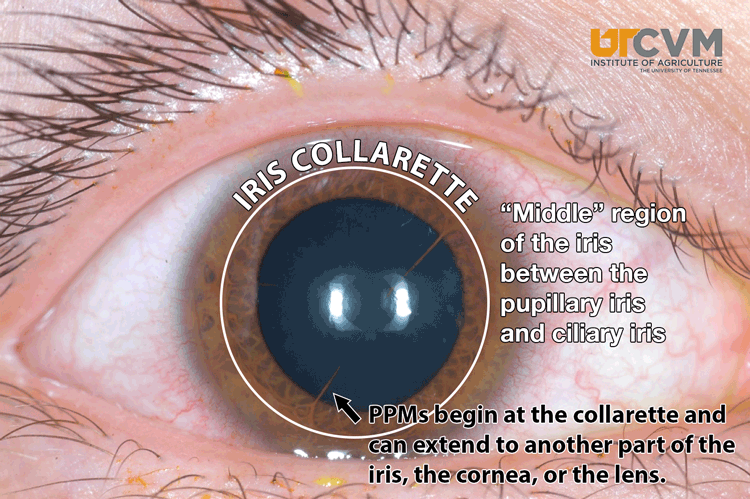
Strand(s) of tissue that extend from the iris collarette to the lens,
cornea, or another area on the iris
Occurrence
Any species - most commonly the dog. Inherited in Basenjis and Corgies
Treatment
None needed
# Heterochromia iridis
Definition
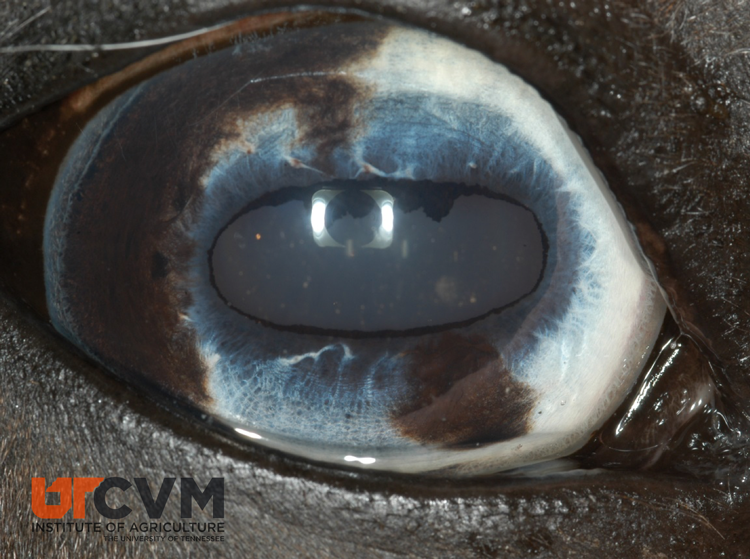
Multicolored iris. Usually seen in animals with dilute coat colors.
These animals often lack fundic pigment, may lack tapetum.
Treatment
None, do not confuse with a melanoma
# Anterior Uveitis
Definition
Breakdown of the blood ocular barrier (via inflammation or another
process).
# Clinical Signs
Aqueous flare/hypopyon/keratic precipitates/fibrin clots - leaking of cells and protein from uveal vessels. In order to maintain its optical clarity, aqueous humor is normally a relatively low-protein fluid. The higher the protein content of a water-based fluid the murkier the fluid. Normally there is an intact blood aqueous barrier in the iris and ciliary body (much like the blood brain barrier) that keeps protein out of the aqueous humor. When these tissues are inflamed, they don’t perform these functions properly and proteins and sometimes cells are allowed to enter the aqueous, resulting in a turbid aqueous humor.
When one shines a FOCUSED LIGHT SOURCE (such as the circle in a direct ophthalmoscope) into the eye from the front and observes from the side, the beam of light traversing the anterior chamber will be visible if it contains appreciable quantities of protein. This phenomenon is called aqueous flare, and for all practical purposes is pathognomonic for anterior uveitis. Flare is subjectively graded on a 1 – 4 scale (1=you can barely see it; 4=it’s so dense it obstructs your visualization of the iris).
Miosis - due to prostaglandin released from the inflamed tissues acting on the sphincter muscle causing it to constrict. Frequently with mild uveitis miosis will not be apparent until resistance to mydriatics is seen. In addition to having acetylcholine receptors for parasympathetic neurotransmission, the pupillary sphincter is loaded with PG receptors, and activation of these receptors results in intense miosis.
Pain - blepharospasm, photophobia, enophthalmos, prolapse of the third eyelid, lethargy. Pain is caused by ciliary spasm.
Redness - ciliary flush, episcleral congestion. Episcleral injection usually indicates intraocular disease, usually either anterior uveitis or glaucoma; scleritis will also cause episcleral injection, but this is a relatively rare disorder. It is very common for episcleral injection to cause conjunctival injection from contiguous inflammation, but the opposite is not true. Thus, dogs with anterior uveitis or glaucoma frequently have episcleral and conjunctival injection, but dogs with conjunctivitis associated with KCS will not have episcleral injection.
Corneal edema - from inflammatory cells damaging endothelium.
Decreased intraocular pressure - due to decreased aqueous production from the ciliary body. Inflammation decreases the ability of the ciliary body to produce aqueous and there is also increased non-conventional outflow from dilated leaky vessels.
Synechia - iris sticking to lens (posterior) or iris sticking to cornea (anterior). Iris adheres with uveitis because fibrin is sticky.

Secondary glaucoma occurs because of iris bombé, or cells in angle. Bombe is the phenomenon in which the pupil becomes synechiaed posteriorly to the lens for 360o, such that aqueous humor cannot flow through the pupil. As a result, aqueous builds up behind the iris, causing it to bow forward. When this happens the peripheral iris synechiaes anteriorly to the cornea, thus obliterating the iridocorneal angle
Cataract formation - abnormal metabolism in the lens due to abnormal aqueous.
Iridial changes - The iris may become darker, congested, and/or swollen. Rubeosis iridis may develop with chronicity.
# General Treatment for Anterior Uveitis
# Goals of treatment
Decrease pain - must stop ciliary spasm
Prevent synechia - must dilate pupil or at least keep it moving
Decrease cellular and protein exudation to prevent glaucoma - use anti-inflammatory drugs.
# Parasympatholytic drugs (see Cornea notes)
Atropine
Tropicamide
# Corticosteroids
MOA
Immunosuppressive
Inhibit arachidonic acid metabolism
Anti-fibrotic
Inhibit neovascularization
General Indications
Inflammatory diseases such as uveitis
Immune mediated diseases
Reduction of neovascularization/scarring in corneal disease
Contraindications
Corneal ulceration
Active infection - if the animal has a systemic disease such as blastomycosis with secondary uveitis, topical steroids can be used, but systemic steroids should be avoided.
Side Effects
Retard corneal epithelialization
Activate latent collagenase
May encourage infection
Topical steroids can have systemic side effects
Best topical preparations for intraocular inflammation are 1% prednisolone acetate and 0.1% dexamethasone. Dosage frequency may initially be q4 hours then decreased to QID. Systemic prednisone is also useful in the treatment of uveitis when the systemic use is not contraindicated.
# Nonsteroidal anti-inflammatory agents:
MOA
Cyclooxygenase inhibition
Indications
Inflammatory disorders when corticosteroids are contraindicated
Adjunct to corticosteroid therapy (especially uveitis)
Topical Preparations
Flurbiprofen
Suprofen
Diclofenac
Generally these drugs are prescribed to be used 3-4 times daily.
Contraindications
- Topical nonsteroidals seem to inhibit healing of corneal ulcers. I don’t look at this as an absolute contraindication for using them on ulcerated corneas, but only use them when necessary.
# Differential etiologies for anterior uveitis
Infection
Blastomycosis, histoplasmosis, other fungal diseases, prototheca, pyometra, Brucella, septicemia, tooth root abscesses, prostatic abscesses, heartworm disease, Rickettsia, RMSF, toxoplasmosis, ICH.
Diagnostics
- Appropriate test for locale and other clinical and physical findings.
Treatment
Treat uveitis with general therapy, and treat primary disease.
Do not put a dog on systemic steroids if you suspect a systemic infectious disease.
Lens-induced uveitis
This is a local immune-mediated cause of anterior uveitis that occurs when cataracts develop to the phase of “hypermaturity,” in which lens proteins liquefy and begin to leak out of the lens capsule. The lens is an immune-privileged site; throughout life, small amounts of lens protein leak out of overwhelming, tolerance is lost, and anterior uveitis ensues.
Diagnostics
- A cataract must be present for lens induced uveitis to occur.
Treatment
- General uveitis therapy. Must get the uveitis under control to do cataract surgery. If the cataract is from acute trauma with puncture to the capsule, must remove lens to save eye.
Secondary uveitis
- Spread of inflammation from the sclera or cornea - most commonly this occurs secondary to ulcerative keratitis.
Neoplasia
Lymphosarcoma, melanoma, ciliary body adenoma, multiple myeloma, etc.
Diagnostics
- Complete physical exam, chest radiographs, and ocular exam.
Treatment
- If the neoplasm is localized to the eye - enucleate. If systemic - treat accordingly.
Trauma Blunt and penetrating trauma can also cause anterior uveitis. Blunt trauma to the eyeball causes inflammation inside the eye by a complex “acoustic interface” mechanism, and penetrating trauma often results in direct damage to anterior uveal structures.
Diagnostics
- History, physical exam, fluorescein stain.
Treatment
- General therapy if no corneal ulcer is present. If an ulcer is present treat appropriately with topical antibiotics. If uveitis is severe one can treat the dog with low dose of systemic prednisone or can try a topical nonsteroidal.
Uveodermatologic syndrome
Autoimmune disease against melanocytes.
Diagnostics
- Depigmentation of skin, nose, uveitis, and chorioretinitis. Most commonly occurs in Akitas, chows, Huskies, and Samoyeds
Treatment
- Immunosuppressive doses of steroids, usually need azathioprine or mycophenolate systemically. Treat eyes with general uveitis therapy. Frequently develop secondary glaucoma or retinal detachments.
Prognosis for vision
- Guarded to poor. Many dogs become blind even with aggressive treatment.
Cardiovascular::
Systemic hypertension (i.e., high blood pressure)
Diagnostics
- Blood pressure measurement with blood work and urinalysis.
Treatment
- Generally treated with enalapril or amlodipine.
Idiopathic (most likely immune-mediated)::
- In the cat idiopathic uveitis is very common, it the dog, however, a cause is more frequently found if diagnostics are pursued.
# Summary
All uveitis cases need a complete history and PE, many cases need complete blood work, titers, chest films and lymph node aspirates if indicated. Treat eyes locally and use systemic therapy where indicated.
# Hyphema
Blood in the anterior chamber (clotted or free)
Complications (same as anterior uveitis)
Synechia
Cataract
Secondary glaucoma
Retinal detachment
Phthisis bulbi
Etiologies
Trauma - blunt or penetrating, post-operatively
Intraocular neoplasia
Blood dyscrasias - leukemias, polycythemia
Clotting abnormalities - Von Willebrands, dicoumarin, liver dz., DIC, warfarin, IMT
Circulatory disorders - hypertension, hyperviscosity
Infectious diseases - RMSF, ehrlichiosis
Retinal detachments
Any disease that can cause uveitis
With so many varying differentials the history and physical are probably the two most important diagnostics. From those one can determine whether to pursue CBC, Panel (which are usually indicated unless the cause is very obvious), chest rads, coagulation panel, titers.
One of the most valuable tools is ocular ultrasound - it can show masses, retinal detachments and lens luxations. It probably diagnoses 75-85% of our cases of hyphema.
Treatment
- Treat the primary disease if one is present. Also treat the eye for anterior uveitis. Fresh blood does not tend to cause glaucoma as the cells are malleable, but as the cells age they lose the malleability. So watch for glaucoma.
Prognosis
- If the hemorrhage is localized to the anterior chamber generally the prognosis is pretty good. However, if hemorrhage is present in the vitreous secondary retinal detachment occurs commonly (or the detachment may have led to the hemorrhage which carries a poor prognosis).
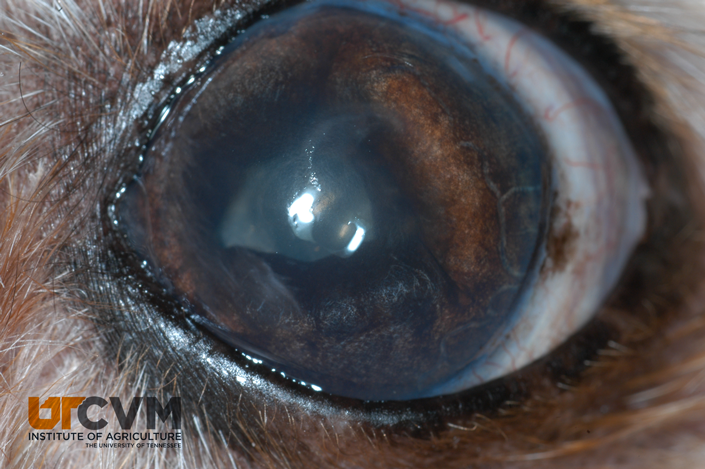
# Iris atrophy
This is a senile, degenerative change in which the iris musculature (sphincter and/or dilator) atrophies, resulting in the holes seen in the iris or an irregular pupillary margin. Because of sphincter atrophy, the pupil may not constrict normally leading to poor PLRs. Iris atrophy is completely benign, and causes no observable functional visual deficits. This is extremely common in older dogs, and is probably the most common cause of poor PLRs in dogs.
Therapy
- None - sunglasses?
# Iris Masses
# Differential etiologies
Iris cysts
Cysts that originate from iris or ciliary body epithelium. The 2 most caudal layers on the iris are the iris myoepithelial layer and the posterior pigmented epithelium. Embryologically the separation between these layers is a potential space, and cyst formation in this space is extremely common. Some believe that these cysts actually form in utero, but just do not become clinically evident until later in life as they grow. Because the cysts originate on the posterior surface of the iris, they are usually not visible until they become large enough that they break free and float into the anterior chamber. They are benign.
Appearance - These are spherical and appear hollow when transilluminated and can be free- floating, attached to pupillary margin or settled out in the iridocorneal angle. Cysts can adhere to corneal endothelium and rupture leaving a dark circle of pigment.
Treatment
- None necessary. May be aspirated if interfering with vision.
Iris Nevis
Darkly pigmented focal lesion on iris face.
Treatment
- None necessary. Must monitor these as some may be preneoplastic.
Uveal tumors
Iris melanomas can be darkly pigmented or amelanotic. Ciliary body adenomas or carcinomas may also occur and are typically pink vascularized masses. Iris melanomas are very rare to metastasize in the dog. Ciliary body adenocarcinomas are more likely to metastasize. Keep in mind that secondary tumors may occur in the eye. Tumors cannot be transilluminated, are not free-floating and are not spherical. Uveitis may occur with a tumor secondary to leaky blood vessels.
Treatment
- If the tumor is a melanoma, it may be okay to watch it unless it starts to grow rapidly. Some tumors may respond to laser therapy. Usually enucleation is warranted.